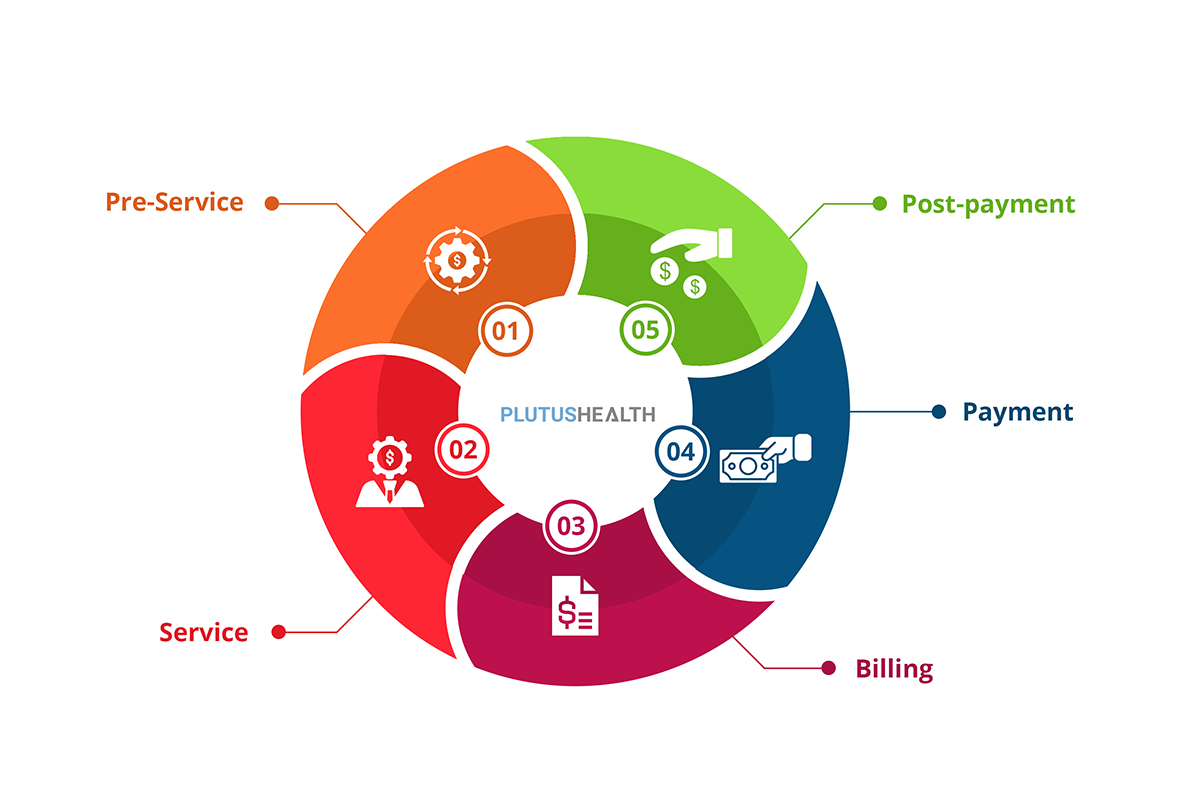
Revenue Cycle Services
EI RCM offers a comprehensive range of revenue cycle services designed to streamline operations, maximize efficiency, and enhance financial outcomes for healthcare organizations
Front-End Revenue Cycle Services
- Patient Scheduling and Appointment Management: Simplify the scheduling process for both providers and patients. Our system ensures smooth operations, high patient satisfaction, and reduced no-show rates through automated reminders.
- Patient-Centric Approach: Prioritizing the well-being of patients through empathetic care coupled with exceptional service delivery—ensuring satisfaction at every touchpoint.
- Eligibility Verification & Benefits Checks: Ensure accurate coverage determination before services are rendered. This proactive approach reduces claim denials and financial burdens on both patients and providers.
- Prior Authorization Services: Expedite authorization processes by managing requests efficiently. We ensure compliance with payer requirements while facilitating timely care delivery for patients.
- Patient Registration/Patient Demographics:Streamline data collection and verification processes to maintain accurate patient records. Our systems minimize errors during registration, enhancing the patient experience from the outset.